APT: Meningitis
This week we will be reviewing Meningitis. The required reading this week are from the IDSA guidelines for Meningitis. We have introduced some essential readings as well, these are aimed to help you master the topic but are not required. Finally, for those that are interested we included the NEJM study regarding use of steroids.
Required Reading
Essential Reading
Optional Reading
APT: Anemia
This week we will be reviewing a big topic Anemia. In preparation we have three short articles covering 3 different categories of anemia. Please read them in preparation of your half day.
APT: Hypertension
This week we will be looking at hypertension and how to diagnose it from outpatient to hypertensive emergency inpatient. In preparation there is a quick 2 page graphic review of the JNC-8 guidelines. There is also a NEJM on intensive vs liberal BP control. As optional reading there is an article from AFP on the JNC8 guidelines.
Optional reading
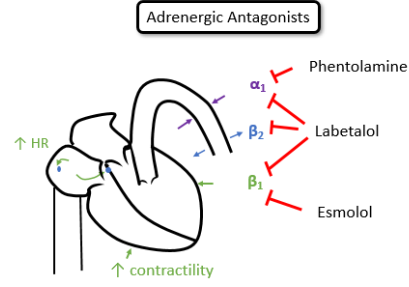
Hypertension
Definitions:
Normal: SBP <120 and DBP <80
Elevated: SBP 120-129 and DBP <80
Stage 1 HTN: SBP 130-139 or DBP 80-89
Stage 2 HTN: SBP ≥ 140 or DBP ≥90
End Organ Damage
Brain - stroke sequelae, multi-infarct dementia
Eye- retinopathy, hemorrhage, papilledema
Heart - diastolic dysfunction, LVH, obstructive cardiomyopathy, HFpEF, coronary atherosclerosis, MI, HFrEF
Kidney- CKD, Albuminuria, reduced GFR, end stage kidney failure
Vascular - aortic aneurysm (ascending, descending), atherosclerotic occlusive disease with limb or organ ischemia, aortic dissection
Hypertensive emergency: BP >180/>120 with evidence of end organ damage
Special Considerations
IPH/SAH - SBP goal < 140 ASAP
Aortic dissection: SBP <120 ASAP
General principals:
1st Hour: decrease BP < 25%
4-6 hours: BP < 160/100
>24-48 hours: BP < 140/90
APT: Diabetes
This week we will be covering diabetes mellitus in AHD.
In preparation of the day you will review the landmark trial RABBIT-2, as well as a retrospective review explaining why we do what we do in the inpatient setting. In addition you will read a review on oral diabetic agents available to help complete your knowledge for when you look to transition a patient to outpatient medications.
APT: HIV and AIDS
This week we will tackle a big topic in the Internal Medicine field. In preparation you will read an article regarding the management of HIV. In addition, there is an article reviewing PCP. For those that want additional information articles have been attached regarding Toxoplasmosis, Cryptococcus, and guidelines from AIDSinfo.
Optional Reading
APT: GI Bleed
The dreaded GI bleeder… This week we will be discussing management of upper GI bleeding. In preparation you will review an article discussing peptic ulcers as the cause of bleeding. In addition there is a study looking at liberal vs conservative transfusion guidelines and the best way to administer PPI for those with GI bleeding.
APT: Acute Kidney Injury
For weeks 13 and 14 of our academic half day we will be splitting the groups up between acute kidney injury and POCUS. For those that are doing Acute Kidney Injury we ask you to review an article from the NEJM. We also included optional reading from the Choosing Wisely series.
Optional Reading:
APT: Antibiotics
This week we will be covering a bread and butter topic every internist needs to know about antibiotics. In preparation we have pulled two of the IDSA guidelines to review. First is the IDSA skin and soft tissue infection guidelines which most of you should be familiar with. Please review the material in this article (you don’t need to read it cover to cover). In addition, we have provided the IDSA guidelines on cystitis and pyelonephritis. We look forward to fighting some bugs with you on Friday!
APT: Endocarditis
This week we will review Endocarditis. In preparation we are asking you to read the JAMA review of the AHA guidelines. As well as a NEJM Review on Native valve endocarditis. Finally the last article is a review on a specific population at risk of infective endocarditis, IV drug users. Included in the material is also the AHA guidelines for Endocarditis. It will help you to review and be familiar with these guidelines but you’re not required to read the document in its entirety.
APT: Liver
This week we will be discussing the Liver and Bile Collecting system. Please review NEJM review articles on cirrhosis and acute liver failure. In addition we are asking you to review ACG clinical guidelines for LFT interpretation/work up.
Approach to Liver chemistries:
ALT: 33 (males), 25 (females), ALP: 115 (males), 100 (females)
Hepatocellular: ALT and AST both up
Cholestatic: ALP up and also direct hyperbilirubinemia
Infiltrative: ASLT up without significant bilirubin or AST or ALT elevation
Non-hepatic: Isolated AST elevated, indirect hyperbilirubinemia
Any degree of AST/ALT elevated:
meds/toxins (aceteaminophen, certain abx, INH, MTX, NSAIDs, heparin, amiodarone, steroids, augment, sulfa drugs, allopurinol, etc)
Alcohol related (alcoholic hepatitis usually >2:1 AST:ALT ratio)
viral infections (Hep A-E, EBV, CMV, VZV, HSV)
Sepsis /ischemia
Biliary obstruction (mixed picture)
NAFLD (usually AST and ALT elevated but <4x ULN)
If above: Workup includes, but not limited to:
stop offending medications/toxins
viral hepatitis serologies
RUQ US (steatosis, cirrhosis, fibroscan)
ANA, ASMA, LKM-1, IgG, Ceruloplasmin, urinary copper, Fe/TIBC >45%, ferritin >200,
Extreme elevation (AST/ALT >1000s, indicates some acute process)
Ischemia (Shock, cardiac arrest, Budd-Chiari, usually AST/ALT goes up first then bilirubin increases)
Meds/toxins (acetaminophen toxicity)
Acute viral infection (Hep A-E, consider HBV reactivation)
autoimmune hepatitis
acute biliary obstruction
If above, workup includes, but not limited to
INR, assess for hepatic encephalopathy, acute liver injury/failure
stop offending meds/toxins, consider activated charcoal, N-acetylcysteine
viral serologies
RUQ US with dopplers
Cholestatic injury pattern (Increased ALP and biliriubin)
Biliary obstruction (Choledocholithiasis, malignancy, primary sclerosis cholangitis, chronic pancreatitis w/ strictures)
intrahepatic cholestasis: Medications (penicillin, cephalosporins, anabolic steroids, bactrim, TPN, sepsis, primary biliary cholangitis (PBC)
If above, workup with include, but not limited to
RUQ US for obstruction
MRCP or ERCP
+/- liver biopsy
Infiltrative pattern (primarily ALP elevation)
sarcoidosis or other granulomatosis (Tb)
Malignancy (lymphoma, mets to liver, HCC)
Amyloidosis
abscess
If above, workup includes, but not limited to
GGT, imaging with RUQ US or CT, MRCP
Consider SPEP + IgG4
+- liver biopsy
Acute Liver Failure
King’s College Criteria
Acetaminophen induced liver failure: pH <7.3, or ALL 3 of INR > 6.5, Cr > 3.4, grades 3-4 Hepatic encephlopathy
All other causes of ALF: INR >6.5 OR 3/5 of the following: age <10 or >40, Tbili >17, INR >3.5, time from jaundice to encephalopathy >7d, unfavorable etiology (Seronegative hepatitis, DILI, Wilson’s)
Decompensated Cirrhosis