APT: Liver
This week we will be discussing the Liver and Bile Collecting system. Please review NEJM review articles on cirrhosis and acute liver failure. In addition we are asking you to review ACG clinical guidelines for LFT interpretation/work up.
Approach to Liver chemistries:
ALT: 33 (males), 25 (females), ALP: 115 (males), 100 (females)
Hepatocellular: ALT and AST both up
Cholestatic: ALP up and also direct hyperbilirubinemia
Infiltrative: ASLT up without significant bilirubin or AST or ALT elevation
Non-hepatic: Isolated AST elevated, indirect hyperbilirubinemia
Any degree of AST/ALT elevated:
meds/toxins (aceteaminophen, certain abx, INH, MTX, NSAIDs, heparin, amiodarone, steroids, augment, sulfa drugs, allopurinol, etc)
Alcohol related (alcoholic hepatitis usually >2:1 AST:ALT ratio)
viral infections (Hep A-E, EBV, CMV, VZV, HSV)
Sepsis /ischemia
Biliary obstruction (mixed picture)
NAFLD (usually AST and ALT elevated but <4x ULN)
If above: Workup includes, but not limited to:
stop offending medications/toxins
viral hepatitis serologies
RUQ US (steatosis, cirrhosis, fibroscan)
ANA, ASMA, LKM-1, IgG, Ceruloplasmin, urinary copper, Fe/TIBC >45%, ferritin >200,
Extreme elevation (AST/ALT >1000s, indicates some acute process)
Ischemia (Shock, cardiac arrest, Budd-Chiari, usually AST/ALT goes up first then bilirubin increases)
Meds/toxins (acetaminophen toxicity)
Acute viral infection (Hep A-E, consider HBV reactivation)
autoimmune hepatitis
acute biliary obstruction
If above, workup includes, but not limited to
INR, assess for hepatic encephalopathy, acute liver injury/failure
stop offending meds/toxins, consider activated charcoal, N-acetylcysteine
viral serologies
RUQ US with dopplers
Cholestatic injury pattern (Increased ALP and biliriubin)
Biliary obstruction (Choledocholithiasis, malignancy, primary sclerosis cholangitis, chronic pancreatitis w/ strictures)
intrahepatic cholestasis: Medications (penicillin, cephalosporins, anabolic steroids, bactrim, TPN, sepsis, primary biliary cholangitis (PBC)
If above, workup with include, but not limited to
RUQ US for obstruction
MRCP or ERCP
+/- liver biopsy
Infiltrative pattern (primarily ALP elevation)
sarcoidosis or other granulomatosis (Tb)
Malignancy (lymphoma, mets to liver, HCC)
Amyloidosis
abscess
If above, workup includes, but not limited to
GGT, imaging with RUQ US or CT, MRCP
Consider SPEP + IgG4
+- liver biopsy
Acute Liver Failure
King’s College Criteria
Acetaminophen induced liver failure: pH <7.3, or ALL 3 of INR > 6.5, Cr > 3.4, grades 3-4 Hepatic encephlopathy
All other causes of ALF: INR >6.5 OR 3/5 of the following: age <10 or >40, Tbili >17, INR >3.5, time from jaundice to encephalopathy >7d, unfavorable etiology (Seronegative hepatitis, DILI, Wilson’s)
Decompensated Cirrhosis
APT: Heart Failure
We will try not to get backed up this week while we discuss heart failure. In preparation you will review the ACC/AHA 2017 Heart Failure Guidelines, and read PARADIGM-HF and an article from JAMA reviewing Heart Failure. For optional reading we have included the EVALUATE-HF and PROVE-HF trials as well as an editorial from JAMA discussing some of the reversibility of remodeling seen with ARNIs.
Optional reading
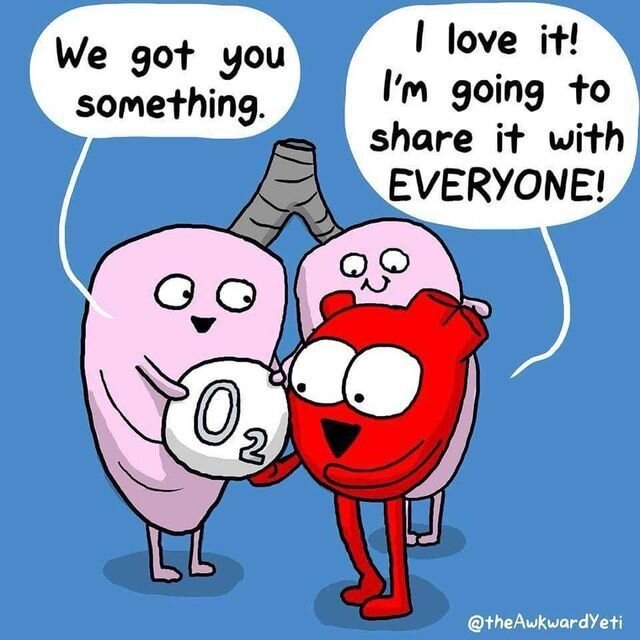
APT: Acute Respiratory Failure
Your patient is short of breath, tripoding on the side of the bed, you’re watching the O2 sat drop. What do you do? This week we hope to help give you additional tools to recognize when someone is in Acute Respiratory Failure. In preparation the required reading is about mechanical ventilation and an outline on acute respiratory failure. If there is time you should read the review article from NEJM on ARDS.
Required Reading
Essential Reading
APT: COPD
On October 22, we will be focusing on COPD for our Academic Half Day. In preparation there is a review article posted for pulmonary function tests. In addition, please review the GOLD Pocket guide. The guide itself is quite long, please focus on the diagnosis and management sections in the guide.
Indications for Noninvasive mechanical ventilation (at least one of the following)
Respiratory acidosis
Severe dyspnea with clinical signs suggestive of respiratory muscle fatigue, increased work of breathing, or both, accessory muscle use (paradoxical motion of abdomen, retraction of intercostal spaces)
Persistent hypoxemia despite supplemental oxygen therapy
SUMMARY
Classification of Airflow limitation severity in COPD
GOLD 1 (Mild): FEV1 ≥ 80% of predicted
GOLD 2 (Moderate): 50% ≤ FEV1 < 80%
GOLD 3 (Severe): 30% ≤ FEV1 < 50%
GOLD 4 (Very severe): FEV1 <30% of predicted
Triple therapy:
IMPACT Trial (Once-Daily Single-Inhaler Triple versus Dual Therapy in Patients with COPD (nejm.org) : phase 3 RCT that compared effects of once daily triple therapy with LABA+LAMA+ICS vs: LABA/ICS or LABA/LAMA on COPD exacerbation
in contrast to FLAME trial which showed a benefit of LAMA-LABA over ICS-LABA for prevention of exacerbations
triple therapy led to significantly lower rates of moderate or severe COPD exacerbations and better lung function and quality of life
Long term supplemental O2 therapy
indicated for stable patients who have SaO2 ≤ 88% or PaO2 ≤ 55mHg
also indicated if PaO2 between 55 and 60mmHg if also evidence of pulmonary hypertension, CHF, polycthemia (Hct > 55%)
NEJM LOTT trial (A Randomized Trial of Long-Term Oxygen for COPD with Moderate Desaturation | NEJM) - patients with stable COPD and resting or exercise induced moderate desaturation, the prescription of long term O2 did NOT result in longer time to death or 1st hospitalization than no long term O2.
APT: Syncope
Academic Half Day will cover classification and management of Syncope.
Prior to attending you will review articles on how to manage syncope and an article specifically reviewing how well physicians can accurately identify cardiac syncope.
APT: Pneumonia
On Friday 9/25 we will be discussing pneumonia. Please read the articles below prior to AHD to help give a good foundation. You are only responsible for the first 7.5 pages of the VAP/HAP guidelines, which is the executive summary, and the CAP guidelines below.
APT: Acute Coronary Syndrome (ACS)
For this week’s Academic Half Day we will review ACS guidelines. In preparation for the day you will review the use of TIMI and GRACE scores with in risk stratification, a review article from NEJM, and an article outlining management from Cleveland Clinic.