APT: Liquid Malignancy
This week we will be covering a rather dense but high yield topic: Liquid Malignancy. Please read Leukemia: An Overview for Primary Care prior to the session. We also included two more in-depth essential readings which you may find helpful.
Pre - Reading
APT: Dermatology
This week we will be looking at rashes. In preparation please review Stanford’s “The General Dermatology Exam” so we will all be familiar with the language prior to the AHD. In addition, there are 3 helpful articles to review about dermatologic emergencies you may see while in the hospital.
Required Reading
Dermatologic Emergencies
APT: Acute Respiratory Failure
Your patient is short of breath, tripoding on the side of the bed, you’re watching the O2 sat drop. What do you do? This week we hope to help give you additional tools to recognize when someone is in Acute Respiratory Failure. Below are some helpful articles and guides that may help you prepare.
Helpful reading
Learner and facilitator guides
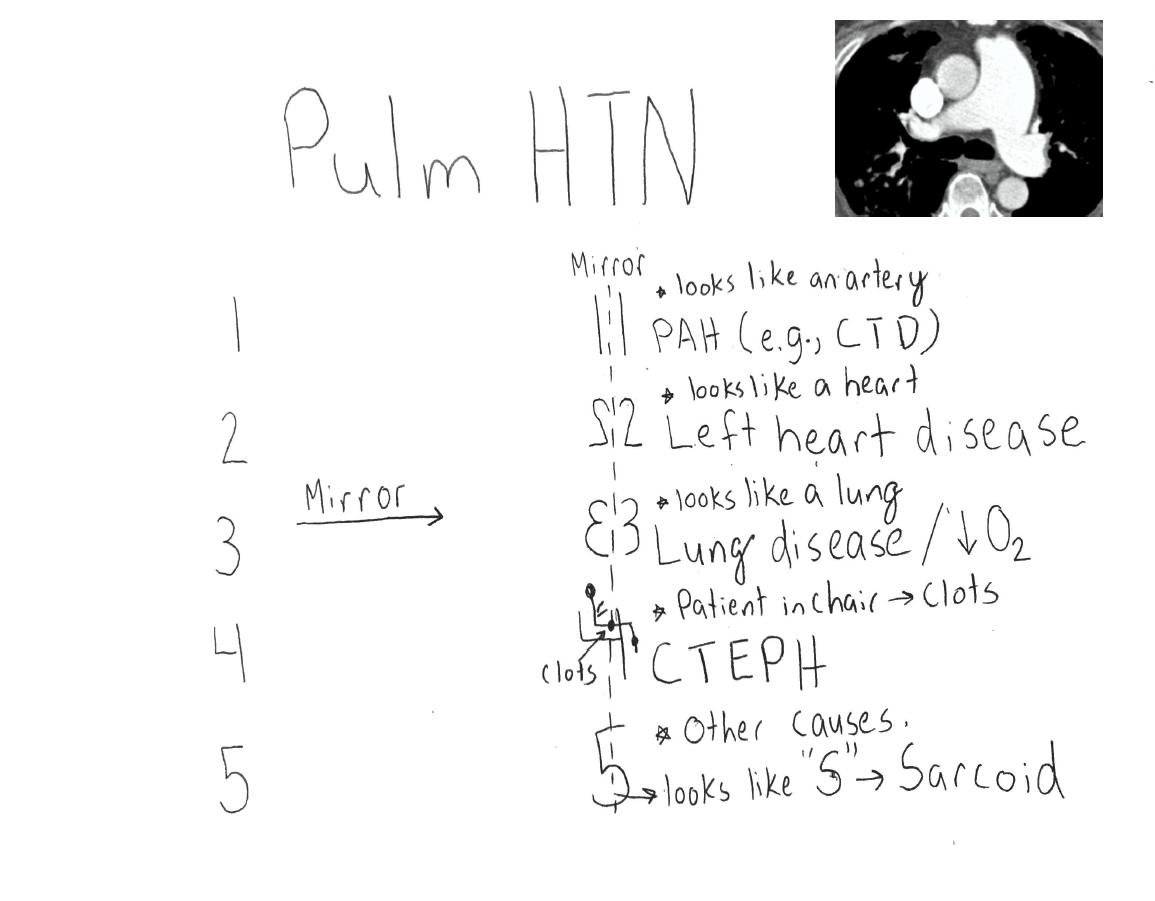
APT: Pulmonary Hypertension
Take a deep breath, it is time to tackle Pulmonary Hypertension. We have included some helpful links below for preparation
Readings
High Yield!
APT: Heme Onc Emergencies
This week we will be covering Heme Onc Emergencies. In preparation, please read the review article below detailing a variety of emergencies that can arise for a patient with a malignancy.
APT: Adrenal and Pituitary
This week we will be discussing the adrenal and pituitary glands. Below are several brief review articles that will help you prepare. It is a lot of reading but will help lay the ground work for understanding some key concepts.
Reading
APT: Meningitis
This week we will be reviewing Meningitis. The required reading this week are from the IDSA guidelines for Meningitis. We have introduced some essential readings as well, these are aimed to help you master the topic but are not required. Finally, for those that are interested we included the NEJM study regarding use of steroids.
Required Reading
Essential Reading
Optional Reading
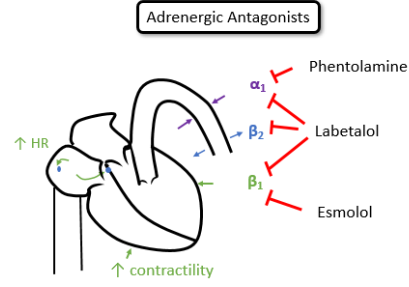
APT: Hypertension
This week we will be looking at hypertension, from diagnosis in the outpatient setting to management in the inpatient setting. Please check out the 2017 ACC HTN guidelines a NEJM article on intensive vs liberal BP control (Sprint Trial). There are additional resources below you may find helpful.
Additional Resources
Hypertension
Definitions:
Normal: SBP <120 and DBP <80
Elevated: SBP 120-129 and DBP <80
Stage 1 HTN: SBP 130-139 or DBP 80-89
Stage 2 HTN: SBP ≥ 140 or DBP ≥90
End Organ Damage
Brain - stroke sequelae, multi-infarct dementia
Eye- retinopathy, hemorrhage, papilledema
Heart - diastolic dysfunction, LVH, obstructive cardiomyopathy, HFpEF, coronary atherosclerosis, MI, HFrEF
Kidney- CKD, Albuminuria, reduced GFR, end stage kidney failure
Vascular - aortic aneurysm (ascending, descending), atherosclerotic occlusive disease with limb or organ ischemia, aortic dissection
Hypertensive emergency: BP >180/>120 with evidence of end organ damage
Special Considerations
IPH/SAH - SBP goal < 140 ASAP
Aortic dissection: SBP <120 ASAP
General principals:
1st Hour: decrease BP < 25%
4-6 hours: BP < 160/100
>24-48 hours: BP < 140/90
APT: Diabetes
This week we will be covering diabetes mellitus.
Below are some helpful articles. Please check out the land mark trial RABBIT-2, as well as a retrospective review explaining why we do what we do in the inpatient setting (Krinsley). In addition there is a review on oral diabetic agents and a short article on the use of sliding scale as monotherapy you may find helpful.
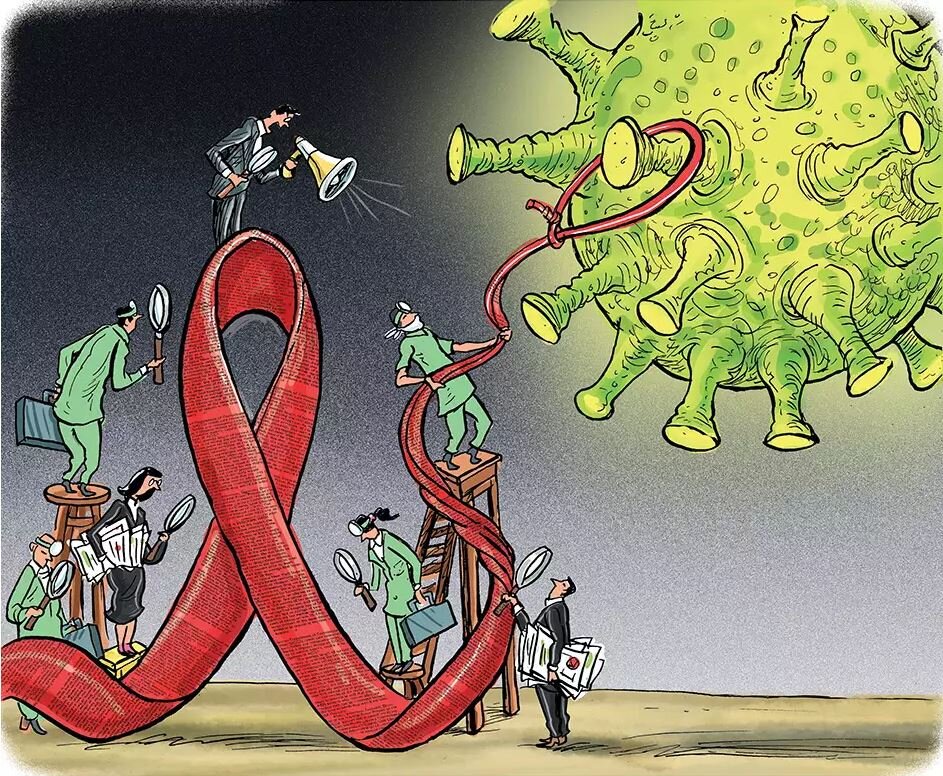
APT: HIV and AIDS
In preparation for this Friday’s APT, please read the below articles on HIV management, PCP, and a review from The Lancet. For those that want additional information, articles have been attached regarding Toxoplasmosis, Cryptococcus, AIDS info guidelines, and an article from NJEM. The Four Decades article is a short read, and the AIDS info recs is a short read if checking the highlighted sections.